Bariatric food, an integral component of post-operative care for bariatric surgery patients, embarks on a journey of nutritional discovery, addressing specific dietary needs and paving the path towards long-term weight management.
Delving into the intricacies of bariatric nutrition, this guide unravels the complexities of macronutrient distribution, food consistency, and meal frequency, empowering patients with the knowledge to navigate their dietary landscape with confidence.
Bariatric Food
Bariatric food is specially designed food for individuals who have undergone bariatric surgery, which is a surgical procedure to treat obesity. It is a crucial part of post-operative care, helping patients adjust to their new digestive system and dietary needs.
Prevalence of Bariatric Surgery
Bariatric surgery has become increasingly common worldwide. According to the American Society for Metabolic and Bariatric Surgery (ASMBS), over 250,000 bariatric surgeries were performed in the United States in 2021. This number is expected to rise as the prevalence of obesity continues to increase.
Role of Bariatric Food
Bariatric food plays a vital role in post-operative care by:
- Providing adequate nutrition: Bariatric surgery reduces the size of the stomach, limiting food intake. Bariatric food is designed to be nutrient-rich and calorie-dense to ensure patients receive the necessary nutrients.
- Promoting healing: Bariatric food is typically soft and easy to digest, reducing strain on the digestive system and promoting healing.
- Managing complications: Bariatric food can help manage complications such as dumping syndrome, a condition that occurs when food moves too quickly from the stomach to the small intestine.
Nutritional Considerations: Bariatric Food

Nutritional requirements for bariatric patients are unique and require careful attention to ensure optimal health and recovery. This includes adequate protein intake, hydration, and a balanced intake of vitamins and minerals.
Protein is essential for building and repairing tissues, maintaining muscle mass, and supporting immune function. Bariatric patients require higher protein intake than the general population, typically 60-80 grams per day, to compensate for the reduced food intake and prevent muscle loss.
Vitamins and minerals are also crucial for overall health and well-being, and bariatric patients may require supplementation to ensure they meet their daily needs.
Macronutrient Distribution and Calorie Intake
Macronutrient distribution and calorie intake should be tailored to individual needs and goals. Typically, a post-bariatric diet includes:
- Protein: 30-40% of total calories
- Carbohydrates: 40-50% of total calories
- Fat: 20-30% of total calories
Calorie intake varies depending on factors such as weight loss goals, activity level, and individual metabolism. Bariatric patients should work with their healthcare team to determine the appropriate calorie intake for their specific needs.
Hydration is also vital for bariatric patients, as they may experience increased fluid loss due to changes in their digestive system. Aim for 64 ounces of water per day or more, especially in the first few months after surgery.
Types of Bariatric Food
After bariatric surgery, patients must follow a specific diet to support their recovery and long-term weight loss goals. This diet includes various types of food, each tailored to the patient’s stage of recovery.
Progression of Food Types
In the early stages after surgery, patients typically consume pureed foods. As they recover, they gradually transition to soft foods and eventually regular foods. The progression of food types is determined by the patient’s tolerance and the healing of their surgical incisions.
Types of Bariatric Food
- Pureed Foods:These foods are blended or mashed to a smooth consistency. Examples include soups, smoothies, and yogurt.
- Soft Foods:These foods are soft and easy to chew. Examples include cooked vegetables, fish, and eggs.
- Regular Foods:These foods are typically eaten by people who have not had bariatric surgery. They include a variety of foods from all food groups.
Supplements and Meal Replacements
In addition to regular food, patients may also need to take supplements or meal replacements. Supplements can help to ensure that patients are getting the nutrients they need, while meal replacements can help to reduce calorie intake.
Meal Planning and Preparation

Meal planning and preparation are crucial aspects of managing weight after bariatric surgery. By following these tips, you can ensure you’re consuming a balanced and nutritious diet that supports your weight loss goals.
Portion Control:
- Use a food scale or measuring cups to ensure you’re consuming appropriate portions.
- Avoid eating directly from containers to prevent overeating.
- Consider using smaller plates or bowls to visually limit your intake.
Food Consistency:
- Start with soft, easily digestible foods immediately after surgery.
- Gradually transition to more solid foods as tolerated.
- Avoid tough, chewy, or sticky foods that can cause discomfort.
Meal Frequency:
- Eat small, frequent meals throughout the day rather than large, infrequent ones.
- This helps prevent overeating and maintains stable blood sugar levels.
- Aim for 5-6 small meals per day.
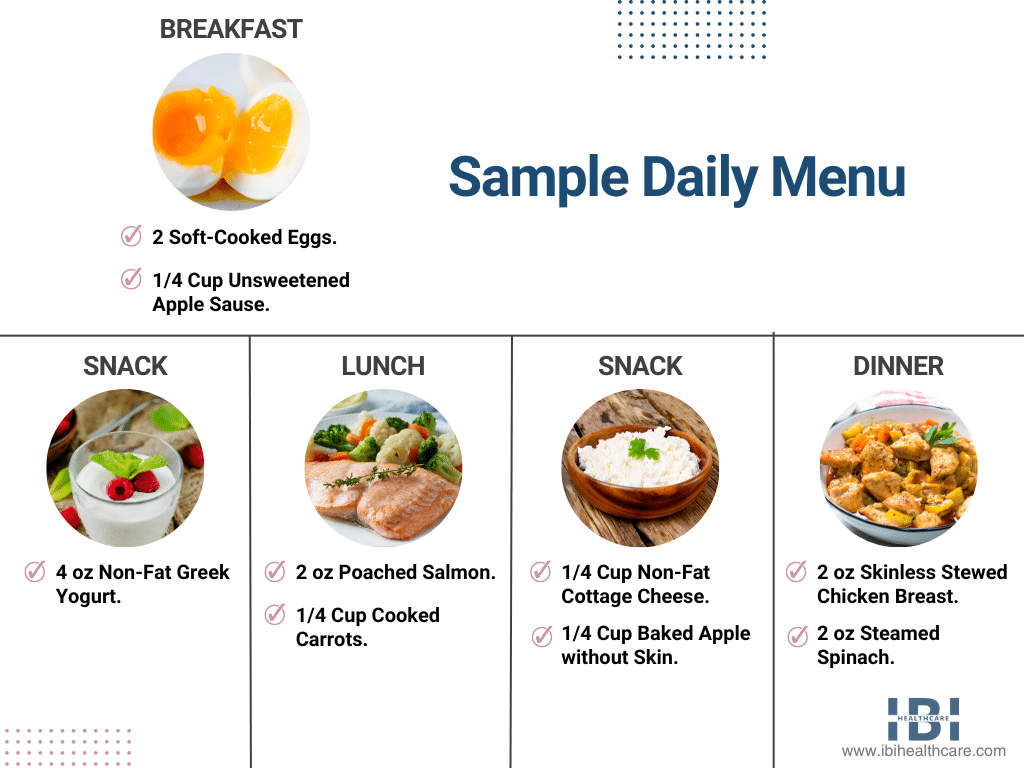
Sample Meal Plan:
- Breakfast:Oatmeal with berries and nuts
- Lunch:Grilled chicken salad with mixed greens and vegetables
- Dinner:Salmon with roasted vegetables and brown rice
- Snacks:Greek yogurt, fruit, or vegetable sticks
Remember to consult with your healthcare team or a registered dietitian for personalized guidance and support in meal planning and preparation.
Challenges and Considerations
Adhering to a bariatric diet presents unique challenges for patients, ranging from physical discomfort to psychological and emotional hurdles. Understanding these challenges is crucial for developing effective strategies to support long-term weight loss success.
One common challenge is the significant reduction in food intake, which can lead to feelings of hunger and cravings. Additionally, the restricted diet may exclude certain foods that patients once enjoyed, leading to feelings of deprivation and dissatisfaction.
Psychological and Emotional Aspects
The psychological and emotional impact of food restriction cannot be underestimated. Bariatric patients may experience feelings of guilt, shame, and anxiety around food, as well as a loss of identity associated with their previous eating habits.
It is essential to address these psychological challenges through therapy, support groups, or other coping mechanisms. Patients need to develop a healthy relationship with food and learn to manage their emotions without relying on food for comfort or emotional regulation.
Overcoming Food Cravings and Managing Hunger
Managing food cravings and hunger is a significant challenge for bariatric patients. To overcome these challenges, patients should:
- Identify their triggers for cravings and develop strategies to avoid them.
- Eat regular, small meals throughout the day to prevent excessive hunger.
- Choose nutrient-rich foods that promote satiety, such as fruits, vegetables, and lean protein.
- Engage in regular physical activity to reduce stress and improve mood.
Maintaining Long-Term Weight Loss
Maintaining long-term weight loss after bariatric surgery requires sustained effort and lifestyle changes. Patients need to adopt healthy eating habits, engage in regular exercise, and develop coping mechanisms for managing stress and emotional triggers.
Support groups, therapy, and regular follow-up with a healthcare professional can help patients stay motivated and accountable throughout their weight loss journey.
Role of Healthcare Professionals
Healthcare professionals play a pivotal role in supporting bariatric patients throughout their weight loss journey. They provide essential guidance, monitoring, and support to ensure patients achieve and maintain their health goals.
Medical Doctors
- Provide comprehensive medical assessments and monitor patients’ progress.
- Prescribe medications, if necessary, to support weight loss and manage underlying health conditions.
- Collaborate with other healthcare professionals to develop individualized treatment plans.
Registered Dietitians
- Provide personalized dietary counseling and education to help patients develop healthy eating habits.
- Create tailored meal plans that meet patients’ nutritional needs and support their weight loss goals.
- Monitor patients’ progress and make adjustments to their diets as needed.
Nurses
- Provide ongoing support and education to patients.
- Monitor patients’ vital signs and overall health.
- Administer medications and assist with wound care if necessary.
Regular monitoring, dietary counseling, and lifestyle modifications are crucial for the success of bariatric surgery. Patients should communicate openly and effectively with their healthcare team to ensure they receive the necessary support and guidance throughout their weight loss journey.
Top FAQs
What is the purpose of bariatric food?
Bariatric food is designed to meet the specific nutritional needs of patients who have undergone bariatric surgery, ensuring adequate intake of protein, vitamins, minerals, and hydration while supporting weight loss and overall health.
How long do I need to follow a bariatric diet?
The duration of a bariatric diet varies depending on individual needs and the type of surgery performed. Typically, patients follow a structured diet for several months to a year, gradually transitioning to a balanced and healthy eating pattern.
What are the common challenges of following a bariatric diet?
Adhering to a bariatric diet can present challenges such as food cravings, hunger management, and emotional eating. However, with support from healthcare professionals and a commitment to lifestyle changes, these challenges can be overcome.
